Sac State students, professor developing anti-HIV agents
Goal is to create topical compounds that could prevent transmission of virus
John Ferrannini – The State Hornet
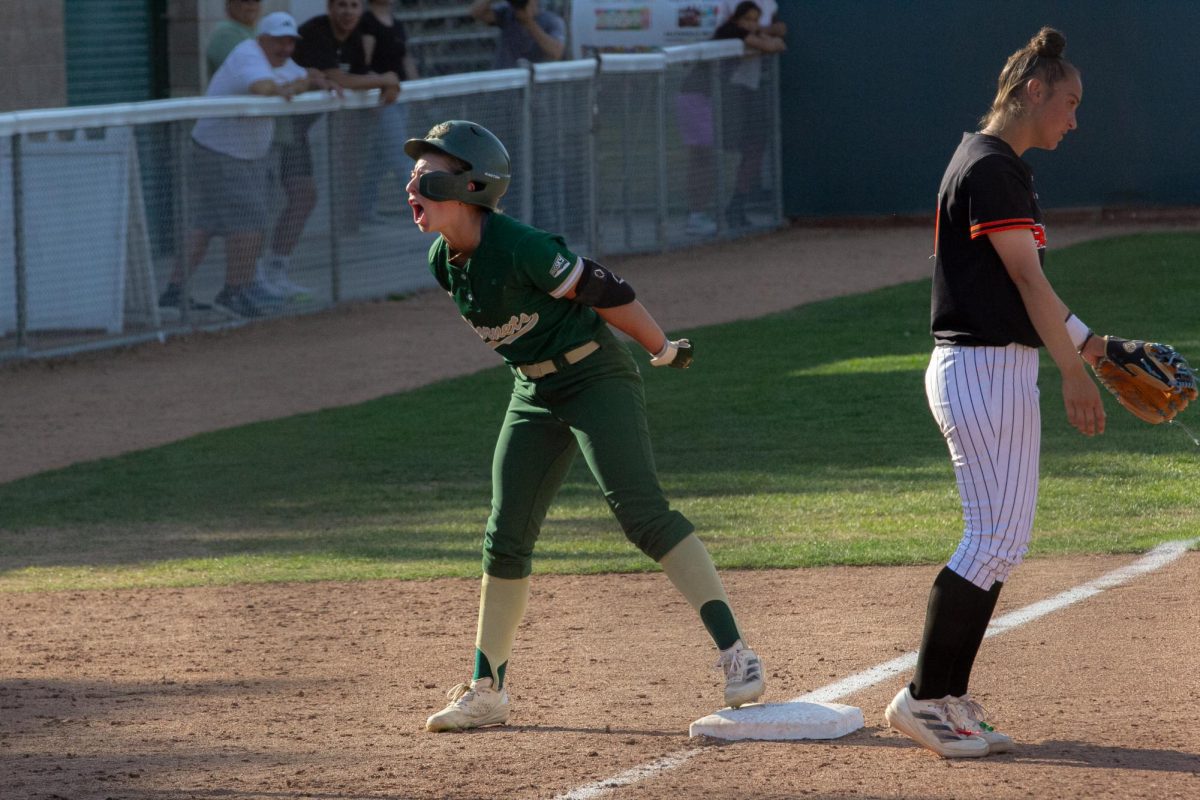
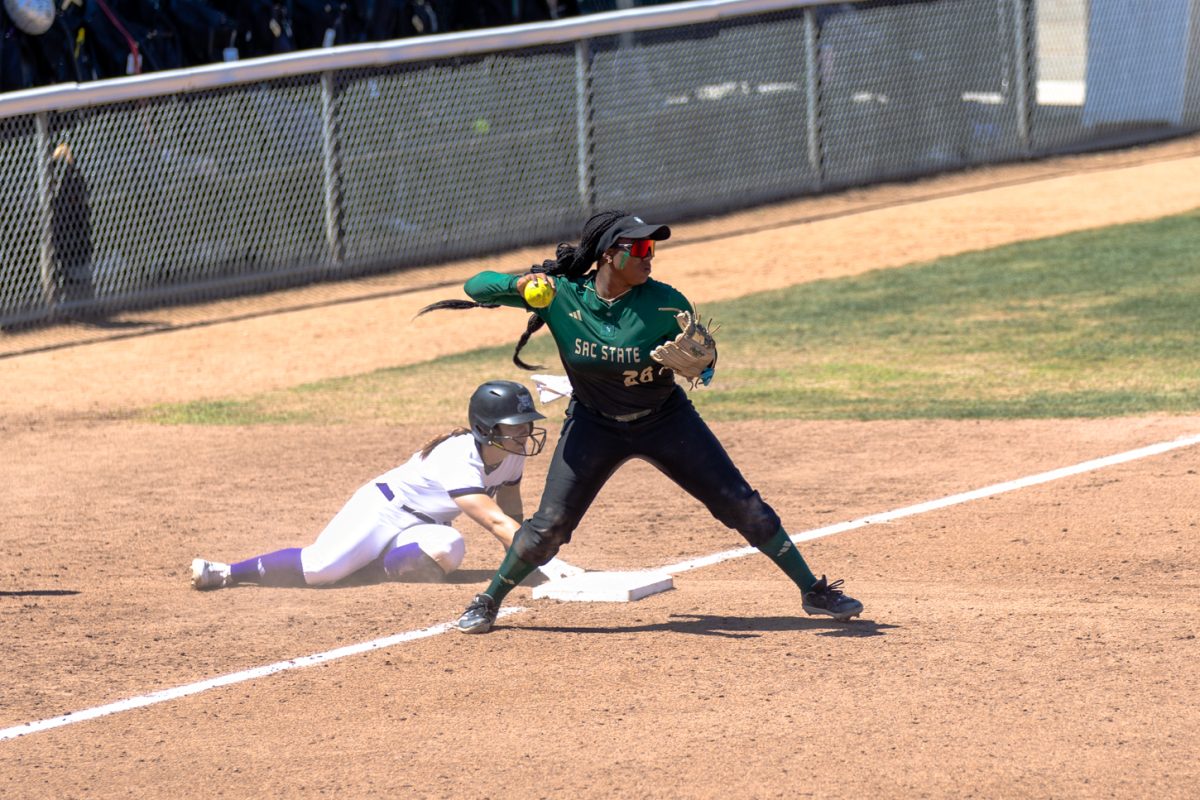
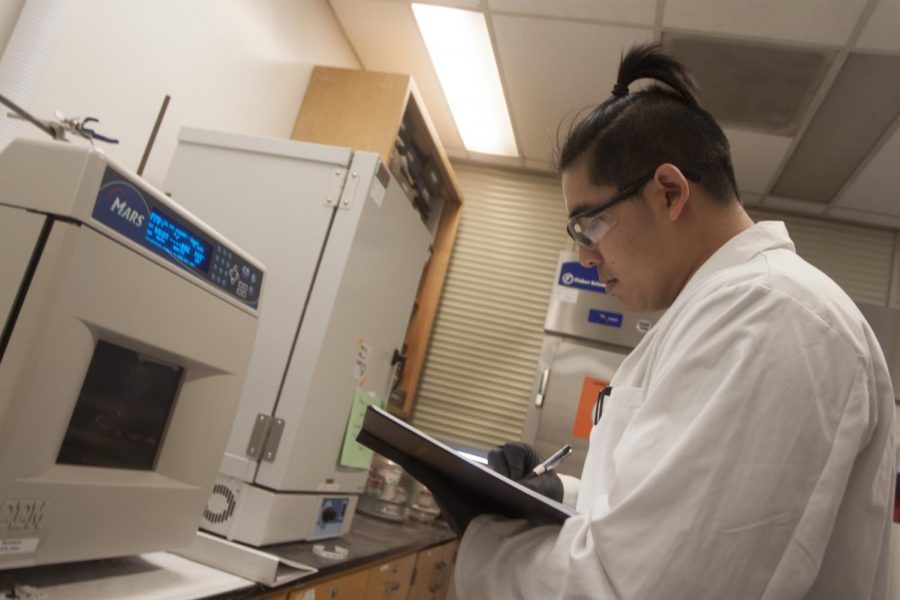
Biochemistry major Kevin Tran uses the microwave in a laboratory on the fifth floor of Sequoia Hall on April 19, 2018 to break down molecules. Tran is working with professor Katherine McReynolds on a project that may yield a topical medicine aimed at preventing the spread of HIV.
Working day and night in a Sequoia Hall laboratory, professor Katherine McReynolds is leading a group of nine Sacramento State students in creating medicine that could be used in the fight against HIV.
So far, the team has synthesized over 20 compounds and have found 10 thus far with properties that could prevent infection with the human immunodeficiency virus if used topically, which they have sent for tests at Duke University with the live virus.
Now, the goal is creating more compounds to strengthen their anti-HIV properties.
“We have started to find what the composition has to be, the size, the number of sugars and now we’re refining the structures in that golden area,” McReynolds said. “The next step is trying to improve the affinity and stability to get stronger interactions.”
How HIV is currently treated and prevented
Infection with HIV is the cause of acquired immune deficiency syndrome, or AIDS.
AIDS destroys the body’s ability to fight disease, leading its victims to die of otherwise rare illnesses that the body’s immune system normally can fight off. These tumors and bacteria — opportunistic infections — are what eventually kills a person with AIDS.
HIV is most commonly spread through semen and blood. The majority of HIV infections in the United States are among men who have sex with men, followed by heterosexual men and women and those who use intravenous drugs, according to the Centers for Disease Control.

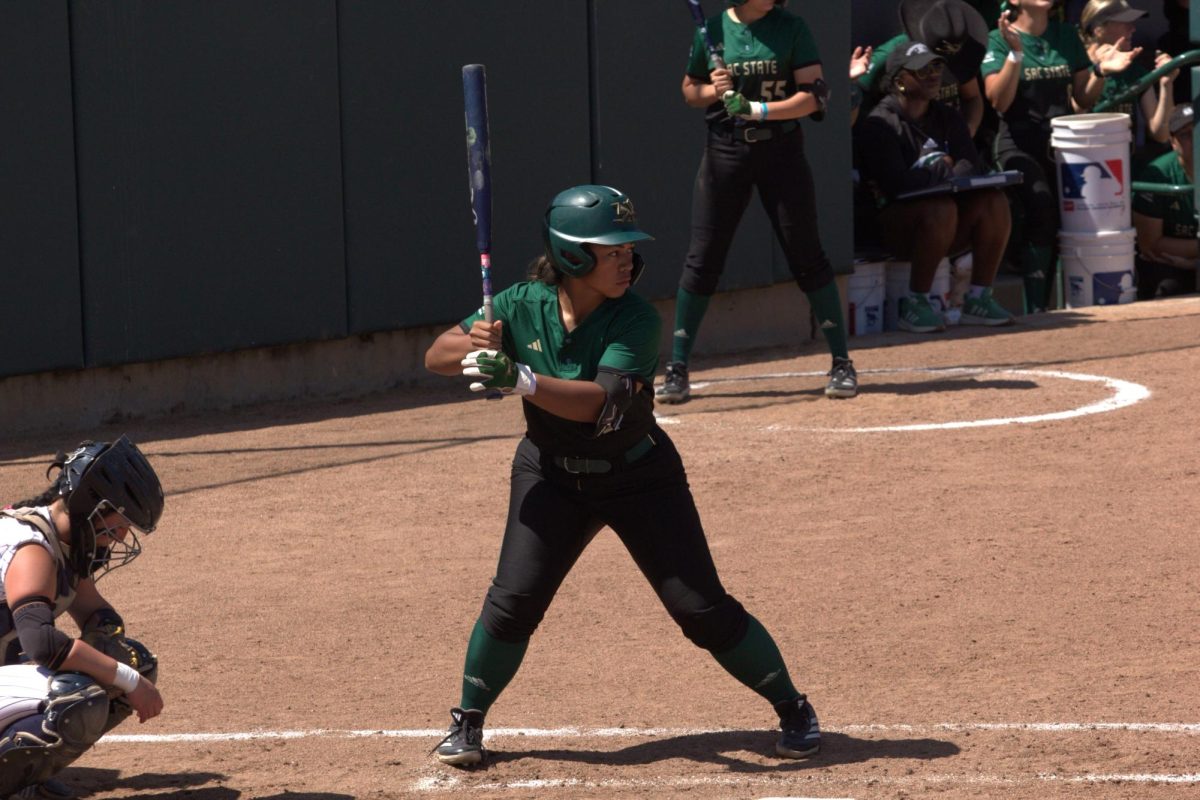
Professor Katherine McReynolds, left, and chemistry graduate student James Carney discuss their work in a laboratory on the fifth floor of Sequoia Hall on April 19, 2018. Cerney is working with professor Katherine McReynolds on a project that may yield a topical medicine aimed at preventing the spread of HIV.
HIV infection is incurable and for the first 14 years after the discovery of AIDS it was considered a death sentence. In the mid-1990s, however, drugs were released that can prevent an HIV-infected person from developing AIDS — dramatically increasing the length and quality of their lives.
In time it was discovered that individuals adhering to these drugs — antiretroviral therapy — cannot transmit the virus to others. It was also discovered that those who are not HIV infected but take a combination of two antiretrovirals can dramatically lower their risk of infection even after unprotected sex with an HIV-positive person.
These drugs combined in a single pill, Truvada, were approved by the Food and Drug Administration for use by non-HIV infected individuals in 2012 for this purpose. The use of a drug to prevent disease in exposed people is called pre-exposure prophylaxis, or PrEP.
A second form of PrEP
McReynolds’ team is trying to create another form of PrEP — one that would be used topically instead of in pill form.
“It would be a chemical barrier,” McReynolds said. “Something that would be topical — maybe inclusion into the lubricant on a condom. There are a lot of different formulations (we can use), like on a vaginal ring.”
The team hopes that the compounds will prevent cells from becoming infected by HIV by containing properties on its surface that will mimic parts of human cells HIV is attracted to.
Instead of binding to human cells, HIV would bind to the compound and then become unable to infect someone.
“It’s a form of molecular mimicry because we’re mimicking what the structures look like on the host cell,” McReynolds said. “We want it in the system long enough for (HIV) to be cleared from your system.”
The team is focusing on a particular protein on the surface of HIV called gp120.
But McReynolds said that the stronger the team can make its compound bond to HIV surface, the better, which is leading them to create compounds with multivalent bonds.
“(HIV) wants the strongest interactions it can get with the host so it can infect it,” McReynolds said. “If there’s initial binding then there will be movement to that area. We’re trying to keep the switch from getting flipped.”
McReynolds said that PrEP and treatment as prevention are the best strategies currently available for HIV prevention, since the nature of the virus makes it particularly hard to vaccinate against in a safe and effective way.
“Mutation is the big issue,” McReynolds said, noting that HIV is like the flu in that it mutates frequently and there are multiple strains in circulation. “They have not found anything that’s effective enough that’d work long-term.”
In fact, HIV has developed some level of resistance to all the drugs that the FDA has approved to treat infected individuals, which leads doctors to often change the regimen of medicines they use to treat HIV-positive people.
Student involvement
There are nine students on the team — six undergraduates and three graduate students. McReynolds said she has trained more than 60 students in total since the project’s inception.
James Cerney, a graduate student of chemistry, said that the project is “challenging.”
“You take basic chemistry from another person’s paper and you think it’s going to work but you change one substituent and it completely alters how it reacts,” he said.
Biochemistry major Lauren Wells, a senior who is graduating in May, said that she is often in the lab when she is not at work or in one of her two classes.
“I took a semester where I didn’t have (McReynolds) for class and my adviser said ‘if you’re going to grad school you should get some research in,’ ” Wells said, adding that those working on the project work six hours a week minimum.
McReynolds, who has been working on the project since 2001, said that the project has been picking up steam.
“We started small and gradually over time (the compounds) have gotten more sophisticated,” she said. “It’s still going to be a while before we have a vaccine but in the meantime we have to prevent as many new infections as we can.”
Your donation will support the student journalists of Sacramento State University. Your contribution will allow us to purchase equipment and cover our annual website hosting costs.